Research has shown that individuals with diabetes have a higher risk of depression than the normal population. Comorbid diabetes and emotional issues are found to be simultaneously associated, with one condition exacerbated by the other and vice versa. Traditional management of diabetes aims at diet, medication, and exercise while the psychological aspect of this disease is often overlooked. Due to negative perceptions and stigma on emotional/mental issues, diabetes patients may even feel reluctant to seek counselling or treatment.
The emotional turmoil of diabetic patients
Studies indicate that individuals with diabetes were more likely to have a strong emotional response to negative experiences. Research also indicates that individuals with prediabetes and Type 2 diabetes had more activity on the right side of their brains, which is associated with depression and negative emotions.
Those with prediabetes and diabetes also recorded lower cortisol levels which shows a lower resistance to stress. It was also found that the occurrence of anxiety in the diabetic patient has been reported as high as 40%.
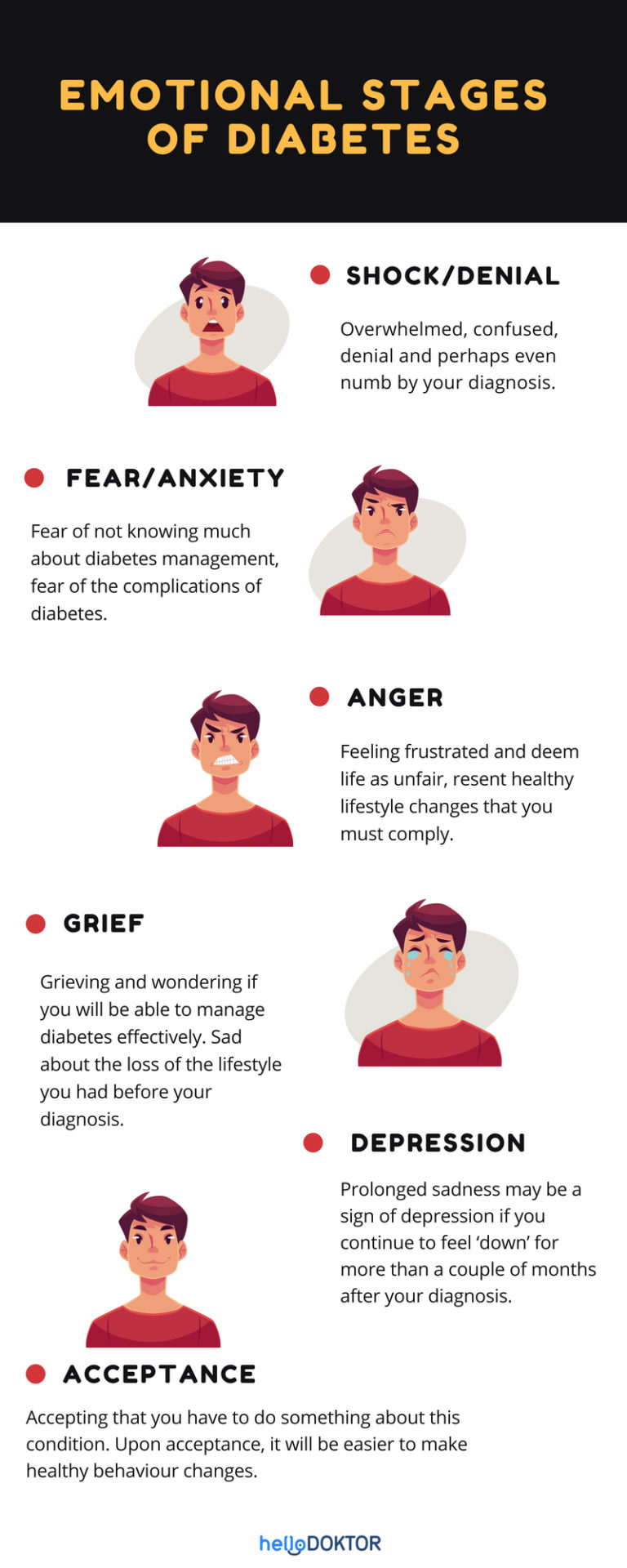
People with diabetes normally go through several emotional stages as they come to grips with having a chronic disease.
Psychological support for diabetes
As diabetic patients become more fixated on negative thoughts, losing weight and managing other health issues can become more challenging. Negative emotions and anxiety affect diabetes self-care management, which is manifested through poorer diet and medication adherence, lesser physical activity, and ultimately higher health care costs.
For healthcare providers, giving the psychological support needed by their patients can make a huge difference in diabetes management. Recent research has shown that when support and care have been given by health care providers, it has resulted in higher perceived self-efficacy and lesser emotional issues with the diabetic patient. With the right support, positive emotional health will facilitate self-management and improved health outcomes. This can be done through:
- Providing awareness and skills development to diabetic patient
- Being more emphatic and improve communication skills
- Personalisation of patients’ management and care according to their needs
- Assess diabetes impact on patients daily routine and how to overcome it
Worries and concerns about diabetes management have caused several patients to impose various restrictions upon themselves. They may isolate themselves, which may precipitate or exacerbate negative emotions. By using an approach that promotes an open discussion about the difficulties in following a diabetes regimen, health care providers can help them gain a sense of freedom through safe self-management skills.
Managing your emotions in facing diabetes
“if you don’t manage your emotions, then your emotions will manage you,” – Deborah Rozman.
Moreover, addressing your emotion should be your priority in diabetic management. Below are some of the steps you can take to manage your emotions:
- Acceptance and acknowledgement
Acceptance and acknowledgement of your condition will help you to focus on strategies to manage this disease. You should also learn to accept and acknowledge the negative emotions that may be surfaced. Overcome them by reframing your thoughts by looking at the situation in a positive way.
For example, a person with diabetes may say to himself, “It’s a good thing I was diagnosed early because it’s not too late for me to start living healthier and to try to reduce my blood sugar levels till they become stable”
- Forgive yourself and grow from this experience
It is easy for one to fall into a trap of guilt, regret and self-blame of their lifestyle consequence. But it is important for us to know that there is no one who is perfect and we should learn to forgive ourselves. Let go and move on to the next step and become healthier.
- Have an action plan
After going through the initial phase of acceptance and awareness, it’s good to move on to the next phase of knowing how to manage diabetes. It would be helpful to go through an action plan involving food and fitness with a friend or a family member.
- Stay connected
Being alone makes diabetes management worse as isolation can make you feel more anxious. Talk to your friends and family for support. Close family members who live with those suffering from diabetes can help by practising similar healthy eating patterns. This can be one of the most powerful ways to support your loved ones by making them feel like they’re not alone in their management plan.
- Relaxation techniques
Try to make time for some peaceful ‘me time’ sessions where you connect with nature in a recluse setting to help you unwind and get away from it all.
Managing diabetes may seem difficult at first but if we stop for a moment and reframe our thoughts and realize that diabetes management actually involves healthy thoughts, healthy emotions and healthy behaviour patterns comprising healthy eating and healthy fitness activities in order to ultimately attain a healthy lifestyle. Shouldn’t everyone be doing the same too? You’re not alone on this journey to becoming a healthier you. We’re all in this together.
This article contributed by Hello Doktor and republished by Voiz Asia upon permission. This article was published in collaboration with Naluri.
By Pamilia Lourdunathan